Lymphatic filariasis or elephantiasis is a neglected tropical vector-borne disease caused by parasitic nematodes such as Wuchereria bancrofti, Brugia malayi, or Brugia timori and spreads through a mosquito bite.
On 1 October 2024, WHO congratulate Brazil for eliminating Lymphatic filariasis as a public health problem.
INTRODUCTION TO LYMPHATIC FILARIASIS
Even after the development of modern medicine, according to WHO, as of October 2024, over 657 million people in 39 countries worldwide remain threatened by lymphatic filariasis. More than 9.7 billion cumulative treatments have been given to stop the spread of this infection since 2000.
Approximately one-third of infections are in India, one-third in Africa, and the remaining third in other parts of South Asia, the Americas, and the Pacific.
This neglected disease results in the abnormal enlargement of body parts and impairment of the lymphatic system, causing considerable morbidity in the infected patients.
WHAT IS THE CAUSATIVE AGENT OF LYMPHATIC FILARIASIS?
Around 90 per cent of lymphatic filariasis is caused by Wuchereria bancrofti, and Brugia malayi, or Brugia timori, account for the other 10 per cent.
After malaria, filariasis is the most common mosquito-borne infection worldwide.
Humans are the only definitive host, and the usual vectors are Anopheles, Culex, Mansonia, and Aedes mosquitoes.
Parasitic nematodes such as Wuchereria bancrofti, Brugia malayi, or Brugia timori are the three types of parasites that result in hydrocele, lymphedema and elephantiasis ( these are pathology terms).
LIFE CYCLE OF LYMPHATIC FILARIASIS
They have biphasic lifecycles where larval development occurs in the mosquito host and adult development in the human host.
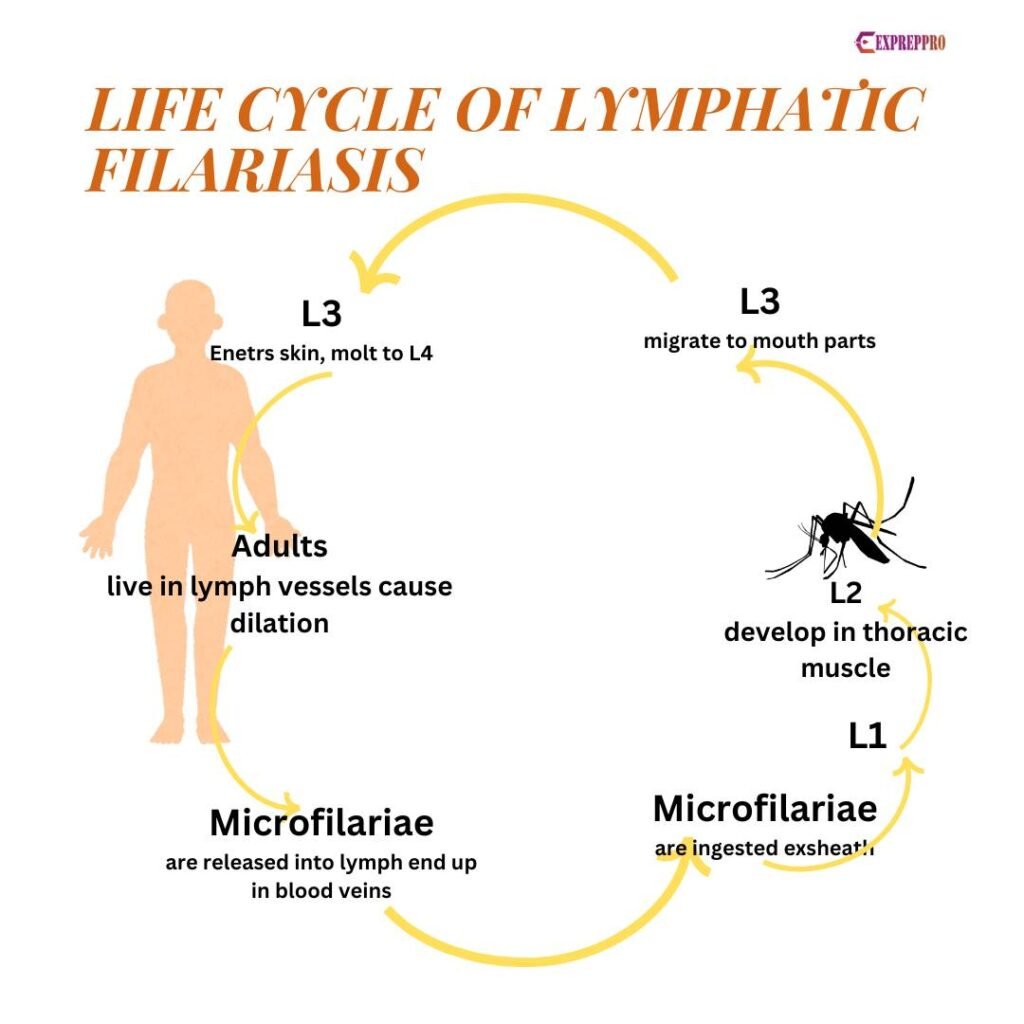
The larvae enter the body as a result of mosquito bites. The infective mosquito passes third-stage larvae to the skin.
Due to ovoviviparous reproduction, first-stage larvae are released from the female. These microfilariae, or first-stage larvae, enter mosquitoes during a blood meal. Once entered, the parasite penetrates the stomach or gut wall and migrates to flight muscles. There, it develops further and later transmits to a vertebrate host.
DEVELOPMENT PERIOD OF LYMPHATIC FILARIASIS
In lymph nodes, these parasites need 3 to 12 months to mature into an adult worm of 10 c.m.
The four larval stages are L1, L2, L3, and L4. Sexually immature adults are called L5 larvae.
Depending on environmental conditions, the L1 to L2 moult need 6 to 10 days. During L2 larvae, the gut develops.
The L2 to L3 moult takes 11 to 13 days, and larvae reach a length of up to 1.6 m.m.
L3 to L4 development occurs in mammalian hosts, and it will take several months (up to 12 months).
WHAT IS OVOVIVPAROUS REPRODUCTION?
In this case, the larvae hatch from the egg inside the uterus and are released from their mother as first-stage larvae or microfilariae.
WHY MICROFILARIAES ARE MORE ACTIVE IN THE NIGHT?
Microfilariae exhibit a surge into the bloodstream at night.
This is due to the low alveolar oxygen tension during the night, and it helps microfilariae to leave the lung’s capillaries and exhibit nocturnal periodicity. It virtually disappears from circulation during the day and will show an increase in the blood between 10 PM and 2 AM.
In some countries like Fiji and Samoa, a strain of Wuchereria with diurnal periodicity has been identified. This is referred to as subperiodic filariasis.
TREATMENT AND PREVENTION
Diethylcarbamazine or Albendazole, in combination with Ivermectin, is used for treatment.
Annual mass drug administration is used to control this disease among the at-risk population.
Vector control also helps to reduce the disease risk.
LYMPHATIC FILARIASIS IN INDIA
This disease has been present in India since the ancient period. 6th-century Susruta Samhita and 7th-century Madhava Nidhana mention Lymphatic filariasis.
The microfilariae was discovered in the peripheral blood by Lewis in 1872 in Kolkata.
Twenty states/U.T. are at risk of this disease. Jammu and Kashmir, Himachal Pradesh, Punjab, Haryana, Chandigarh, Rajasthan, Delhi, Uttarakhand, Sikkim, Arunachal Pradesh, Nagaland, Meghalaya, Mizoram, Manipur, Tripura are free from indigenously acquired infection.
The government of India aims to eliminate lymphatic filariasis by 2027, three years ahead of the global target year. To achieve this goal, the Sarva Dawa Sevan or MDA campaign was launched by MoHFW.
In the last two years, India has seen a decline in vector-borne tropical diseases, especially lymphatic filariasis.
SARVA DAWA SEVAN OR MDA
India’s government plans to eliminate Lymphatic filariasis by the year 2027.
Health workers will go to houses and distribute medicine in ten filaria-affected states with high-burden districts.
These states include Bihar, Chhattisgarh, Jharkhand, Maharashtra, Uttar Pradesh, West Bengal, Karnataka, Odisha, Madhya Pradesh and Andra Pradesh.
This project also aims to increase vector control efforts to eliminate Culex mosquitoes.
HOW DID BRAZIL WIPE OUT LIMPHATIC FILARIASIS?
- To fight against this disease, Brazil developed a national plan in 1997.
- Brazil’s government started an effective vector control programme.
- Effective and successful mass drug administration programme.